Breast Augmentation
Conveniently located to serve the areas of Boulder, CO

Breast Augmentation surgery, or mammoplasty, involves using implants to revitalize breast volume and shape after pregnancy or weight loss. Augmentation is a popular option if you are unhappy with your breast size. By balancing your figure, increasing the wholeness and prominence of your breasts, a breast augmentation also improves your self-image and confidence.
Contents
- 1 Before and After Photos
- 2 Who is a good candidate for breast augmentation?
- 3 Who may not be a good candidate for Breast Augmentation?
- 4 Will Breast Augmentation also work in people with droopy or sagging breasts?
- 5 Am I too old to have Breast Augmentation?
- 6 Should I wait until I am finished having children before having Breast Augmentation?
- 7 Mommy Makeover
- 8 Surgical approaches to Breast Augmentation
- 9 Methods of choosing breast implant size
- 10 Where is the implant placed?
- 11 Rippling of Breast Implants
- 12 Sagging
- 13 Options for Breast Implants
- 14 Preparing for your surgery
- 15 How should I prepare for surgery?
- 16 How long will the surgery take?
- 17 What type of implant will be used?
- 18 After Your Surgery
- 19 What kind of scars will I have?
- 20 Will my breasts look “natural”?
- 21 Will my nipple sensation or feeling change?
- 22 Will having a breast augmentation increase my chances of getting breast cancer?
- 23 Breast Augmentation Surgery Post-Operative Instructions
- 24 When to call
- 25 Possible Complications of Breast Augmentation Surgery
- 26 Breast Implant Massage Exercises
- 27 Schedule your Appointment
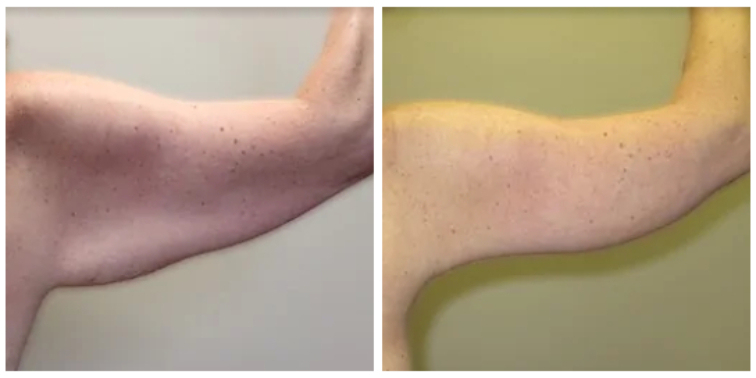
Before and After Photos
Who is a good candidate for breast augmentation?
Candidates must be healthy, have no active diseases or severe, pre-existing medical conditions, and must have practical expectations of the results of the surgery. Typically, patients who gain the most from breast augmentation aren’t content with the current state of their breasts due to an imbalance or irregularity, or women who want to return to their pre-pregancy breast size.
Who may not be a good candidate for Breast Augmentation?
- Women who have serious medical conditions. Prior illness can alter the way the body recovers and can cause problems during or after the procedure.
- Women who have unrealistic expectations regarding the outcome of the surgery. This operation changes only a tiny portion of the body. Though some women report they are content with their new breasts and enjoy their new image, this procedure should not be seen as a solution for unhappiness or difficult relationships.
- Women with a family history of breast cancer should examine this concern with the surgeon.
- Women who have a personal, or family history of numerous breast cysts may not be good candidates for breast augmentation surgery. In these patients, biopsies are often necessary to rule out breast cancer. If needle biopsies are required, damage or deflation is a possible side effect.
- Women who are currently pregnant, or breast-feeding. These women should hold off until they have completed breast-feeding.
- Women who are actively losing or gaining weight. Since weight loss or gain can alter the shape and size of the breasts, a patient should wait until they are at a steady weight prior to receiving breast implants.
- Lastly, women with unstable mental health that may prevent them from following pre/post-operative instructions, or women whose decision is motivated by others.
NOTE: You may not be a candidate for surgery if you smoke, have recently quit smoking, or if you are exposed to second-hand smoke. Primary and secondary smoking decreases blood flow to the body’s tissues. This can result in prolonged wound recovery, skin loss, infection, increased scarring, and numerous other complications depending on the kind of operation performed.
Will Breast Augmentation also work in people with droopy or sagging breasts?
Women with sagging breasts, which is called “ptosis”, can also receive breast implants. Depending on how much the breast sags, an additional surgery may also be necessary. For breasts with nipples that droop below the lower crease of the breast, a breast lift surgery, or mastopexy, is often required as well. This surgery will also add scars around the nipple unlike most breast augmentation surgeries. Without this additional surgery to remove excess skin, placement of the implant can cause the breast to have a “double bubble” look. Commonly, women with sagging breasts often have the implants placed under the breast tissue, or “subglandular” to avoid these problems.
Am I too old to have Breast Augmentation?
The most common patient for this surgery is a woman in her 30’s, and has been considering this operation for many years. Many women in their 40’s and 50’s have undergone breast augmentation surgery with good results.
Should I wait until I am finished having children before having Breast Augmentation?
Pregnancy will change the size and shape of a woman’s breasts whether she has implants or not. These changes may adversely affect the cosmetic appearance of any augmented breast.
It is usually recommended that pregnancy be postponed until 6 months after the surgery. Breast-feeding with implants is still possible and has been shown to be safe for the baby and the mother.
Mommy Makeover
Many women elect to have multiple plastic surgery procedure performed at once. There are many reasons for doing so. First, it costs less than having them performed separately. You will only incur one surgical center expense and only one anesthesia expense. You may also save money on pain medication, if needed. One of the most popular plastic surgery procedure combinations in recent years has been the Mommy Makeover. This procedure involves full body contouring and may be a combination of breast augmentation, tummy tuck (abdominoplasty), and liposuction. It restores youthfulness to the whole body, from your breasts down to your hips.
Surgical approaches to Breast Augmentation

When deciding the type of surgical incision, it is important to remember that each patient’s body is different.
Incisions vary based on the type of implant, degree of enlargement desired, your particular anatomy, and patient-surgeon preference. They are made in inconspicuous areas to minimize visible scarring. You and your plastic surgeon will discuss which incision options are appropriate for your desired outcome. Implant type and size will be determined not just on your desired increase in size but more importantly on your breast anatomy, skin elasticity and body type.
Inframammary
This approach tends to be more direct and to allow greater control of the implant positioning. Seventy to eighty percent of breast augmentations are performed using this incision site. Since the incision is in the fold underneath the breast, the parts of the breast that make milk are less likely to be affected. This option also allows the surgeon to look directly where the implant will be placed and allows for better implant placement. In addition, if complications occur and additional surgeries are needed, the original incision can be used. Some of the other incision sites may not be ideal for treating complications.
This approach works well with patients who have already had children and are a little older, since age creates a small amount of natural sag in the breast. This minimal sag allows the incision to be well hidden in most women. For women who have yet to have children, who are thin, or who are younger, this surgical option may result in a more visible scar.
Trans-axillary
This incision is from the armpit, or the axilla. Fifteen to twenty percent of breast augmentations are done using this surgery. This incision site can be used for both submuscular and subglandular placement of the implant. One of the advantages to this site is placement of the scar in a less visible location. It also allows better access to place the implant in the submuscular position. Some surgeons will also use an endoscope, or a small fiber-optic camera, to help them in this surgery. This approach is often used for thin women where submuscular placement would allow more natural appearance to the breast. It is also used for women who are younger and have little to no breast sag, thus making an inframammary scar more visible.
A potential disadvantage to this approach is that proper implant positioning is somewhat more difficult, particularly if the procedure is performed without and endoscope. In addition, if the patient experiences scar thickening postoperatively, this scar may be visible when the patient wears a shirt or dress without sleeves. In addition, it may be visible when the patient wears a bathing suit and raises her arms.
Trans-umbilical Breast Augmentation (TUBA)
The incision and scar in this newer approach is through the belly button or umbilicus. A fiber-optic camera (endoscope) is tunneled from the umbilicus to a pocket under the breast. The implant is inserted through this tunnel into the breast and is then inflated with saline. It is important to note that using this incision, only sub-glandular placement is possible. Advantages of the TUBA include a less visible scar, and a faster recovery time. Disadvantages of this approach include a slight increase in the likelihood of damage to the implant, and the possibility of tunneling under one of the chest muscles (pectoralis major) during placement. Furthermore, complications that require additional surgeries for treatment may require a new incision closer to the breast. In addition, implant manufacturers frequently will not honor the implant warranty if the implant is placed through this approach.
Peri-areolar
This is an incision around the nipple. The scar usually blends into the edge of the areola. However, since the incision lies closer to the parts of the breast that make milk, women with this type of breast augmentation often have more problems with breast feeding and nipple sensation following the surgery.
Methods of choosing breast implant size
This is often one of the most difficult decisions, and for many reasons, has the most potential for disappointment. Breast implant volumes are often poorly understood by patients, who don’t realize all the variables (ribcage size, chest shape, existing breast volume) that will dictate what a given implant size will do for them. How big your breasts will be after surgery will depend on certain size issues:
- How big your chest is now
- How much breast tissue you have naturally
- What size and type of implant you choose
For instance, women often come with a new bra size in mind. Since bra size depends on many factors, a better choice is to look at before and after pictures. By finding a women with a similar body shape in the “before” picture, and then with the results you want in the “after” picture – misconceptions on the final breast size can be avoided. In addition, we often have our patients wear implants under their bra to decide if this is the size they want.
Where is the implant placed?
The implant can be placed in one of two areas:
- 1Sub-Glandular: When the implant is placed behind the breast tissue Seventy-five percent of breast implants are placed in this position.
- Sub-Muscular: When the implant is placed behind one of the surface chest muscles called the pectoralis major, this is referred to as “submuscular.”
Advantages exist for both sites depending on the shape of the breast before surgery:
- Mammography is generally easier to perform with submuscular breast implantation.
- Studies suggest that placing the implant behind the muscle decreases the risk of scar tissue contracture following the surgery.
- Submuscular placement is also recommended for smaller women, or women who want to greatly enlarge their breasts since this will often give better results.
- If you have little natural breast tissue or desire an implant larger than your natural breast tissue can cover, you may achieve a more natural looking result with either a complete submuscular or partial submuscular placement.
- In most women with average to little breast tissue, under the muscle placement (either partial or complete) can help to avoid the “fake” look of implants.
- If you have a lot of sag or droop, you may require a breast lift (mastopexy) if you elect for either partial submuscular or fully submuscular placement. If you do not get a breast lift at the time of your breast augmentation, the breast implant will align with your chest wall instead of your breast tissue.
- Women who lift a lot of weight (think female body builders) may see distortion with any placement below the muscle because of the strength and flexion of the muscle.
- If you have sag and you do not want a lift, you may be better off having your implants placed over the muscle. The subglandular surgery may give better results for women with sagging or droopy breasts. If you have adequate breast tissue to cover the size breast implant you want, above the muscle placement can give you a very natural look.
Rippling of Breast Implants
If you have little breast tissue, partial submuscular breast implant placement or fully submuscular breast implant placement is likely to reduce the chances of visible rippling of the breast implant. This is because the implant is partially or fully covered by muscle, in addition to breast tissue. The extra padding created by using the muscle to partially or completely cover the implant hides potential rippling beneath a thicker layer of tissue.
Sagging
Many plastic surgeons contend that over the muscle breast implant placement is more likely to lead to sagging as you age. In a complete submuscular placement or a partial submuscular placement, the breast implant may be better supported resulting in less sagging of the augmented breast over the long term.
Options for Breast Implants
Saline implants are filled with sterile salt water. They can be filled with varying amounts of saline which can affect the shape, firmness and feel of the breast. Should the implant shell leak, a saline implant will collapse and the saline will be absorbed and naturally expelled by the body.
Silicone implants are filled with an elastic gel. The gel feels and moves much like natural breast tissue. If the implant leaks, the gel may remain within the implant shell, or may escape into the breast implant pocket.
The method for inserting and positioning implants depends on the type of implant, degree of enlargement desired, your body type, and your surgeon’s recommendations. Incisions are closed with layered sutures in the breast tissue and with sutures, skin adhesive or surgical tape to close the skin. Over time the incision lines will fade. The results of breast augmentation are immediately visible. Over time, post-surgical swelling will resolve and incision lines will fade. Satisfaction with your new image should continue to grow as you recover and realize the fulfillment of your goal for fuller breasts.
Preparing for your surgery
You will be given specific instructions on how to prepare for your surgery. A pre-operative information packet will be provided that explains everything you should do and know before your surgery date. Your surgeon will instruct you on how to prepare for surgery, including guidelines on eating and drinking, smoking, and which vitamins and medications should be taken or avoided. You should arrange for someone to drive you home after your surgery, whether your surgery is done on an outpatient or inpatient basis. You may also want to make arrangements for someone to help you out for a day or two after you leave the hospital.
How should I prepare for surgery?
- Do not take aspirin, aspirin containing products, or ibuprofen (Excedrin, Bufferin, Anacin, Advil) 2 weeks before surgery. These drugs can change how blood clots. By asking your doctor, another drug can be used in its place.
- No food or of drink should be taken after midnight the night before the surgery.
- Do not drink any alcohol within 24 hours of having lab work done or before the surgery.
- Make sure you have someone to take you to and from surgery and to take care of you for 48-72 hours after the surgery.
- For 3 days before the surgery, wash your breasts thoroughly each day with antibiotic soaps such as Safeguard, or Dial.
- Do not wear deodorant, perfume, or powders the day of the surgery.
- Wear comfortable, loose fitting clothes that will button-down, the day of the surgery (sweat pants & button-down shirt). Also wear low heeled, slip-on shoes.
- Wear glasses or bring a contact lenses container.
- Fill all prescriptions given before the surgery.
- Do not start taking your antibiotics until after the surgery, or as directed.
- Remove nail polish and trim the nail of your index finger, since this is where an oxygen monitor will be attached.
- In the car for the ride home have a bucket with a lid in case of nausea from the anesthesia. Also bring your pain medications, and two pillows.
- Arrange care for children and/or pets.
- Lay out all bathroom items prior to surgery – so no excess reaching is necessary.
- Take care of all the little things like bills, gas for the car, laundry, and emptying the garbage before surgery.
- Have easy to eat foods like Jell-O and soup as well as easy to fix foods in places that are easy to reach!
- Though reaching and lifting objects greater than 5 pounds is not allowed after surgery (a gallon of milk weighs 8lbs), patients are encouraged to walk as much as possible. Problems with blood clots in the legs can occur after surgery, and walking can help prevent this.
How long will the surgery take?
Depending on the type of breast augmentation chosen (where the incision in made) the surgery will usually last 1-2 hours.
What type of implant will be used?
Implant Surface – Two implant surface types exist: smooth and textured. The textured surface means the outside of the implant has lots of tiny microscopic bumps. This was developed to decrease a complication called contracture after surgery (discussed in risk section below.) Some studies show a decrease in this complication when using textured implants. In reality, however, many surgeons have excellent results with the smooth implants. Smooth implants also have a softer more natural feel. Since options exist on what type of implant is used, it is important to discuss at your consultation.
After Your Surgery
See post-operative instructions for information about what to expect during your recovery. It is very important that you follow your surgeon’s instructions. This will promote healing and improve progress towards your new physical appearance. Also, it is important that you attend all scheduled follow-up appointments so that your surgeon can assess your long-term results and answer any questions or concerns you may have.
What kind of scars will I have?
Implant Surface – Two implant surface types exist: smooth and textured. The textured surface means the outside of the implant has lots of tiny microscopic bumps. This was developed to decrease a complication called contracture after surgery (discussed in risk section below.) Some studies show a decrease in this complication when using textured implants. In reality, however, many surgeons have excellent results with the smooth implants. Smooth implants also have a softer more natural feel. Since options exist on what type of implant is used, it is important to discuss at your consultation.
Will my breasts look “natural”?
Patient satisfaction for breast augmentation surgery is high. Even women who experience complications after surgery are often satisfied with the way they look. How “natural” post-implanted breasts look will depend on the size of the implant AND the patient. For example, women who have small breasts before surgery and are receiving large implants are less likely to have “natural” appearing breasts, compared with women receiving smaller implants (i.e. more modest enlargement.)
Not all patients are happy with this surgery. Understanding the potential risks for this surgery as well as having realistic expectations will help ensure a good result.
Will my nipple sensation or feeling change?
Most women will have loss of some feeling or sensation following breast augmentation surgery. For most of them, this lasts 6-12 months before returning to normal. Approximately 15% of women, however, have alterations in nipple sensation.
Will having a breast augmentation increase my chances of getting breast cancer?
This is one of the most frequently asked questions by women considering this surgery. Many studies have shown that women who get implants are not at an increased risk for getting breast cancer. In addition, implants do not delay the detection of breast cancer. Numerous studies, as well as evidence from the National Cancer Institute, show that having implants does not hinder the patient or their physician in finding breast tumors. Finally, breast implant patients who do get breast cancer have the same chance of obtaining remission, or being free of cancer for 5 years, as women without implants
Breast Augmentation Surgery Post-Operative Instructions
How Will I Feel After Surgery?
For the first few days after surgery, you will be in pain, and you will be sore. These symptoms are common and shouldn’t cause alarm:
- Pain – which responds well to prescribed medication(s)
- Swelling – which is noticeably reduced after ice is applied
- Soreness – which is concentrated at the chest, neck and back
- Redness – which generally appears near incisions and stitches
- Nausea – which gets better after a snack or sips of ginger ale
Dr. Roesner will typically write prescriptions for related medications prior to surgery. Get them filled in advance and take them as prescribed to keep pain and swelling down. Don’t skip or delay doses because they can take up to 30 minutes to kick in – if you wait until it hurts, you will be in pain.
Some patients experience nausea or a “hangover” response to anesthesia. One way to overcome that is by limiting your movement. Keep a bucket and a moist towel or baby wipes nearby in case you feel sick. That way, you won’t have to make a painful dash for the bathroom.
Post-op Instructions
- Have someone drive you home after surgery and help you at home for 1-2 days.
- Get plenty of rest.
- Follow balanced diet.
- Decreased activity may promote constipation, so you may want to add more raw fruit to your diet, and be sure to increase fluid intake.
- Take pain medication as prescribed. Do not take aspirin or ibuprofen, or any products containing aspirin or ibprofen.
- Do not drink alcohol when taking pain medications.
- Even when not taking pain medications, no alcohol for 3 weeks as it causes fluid retention.
- If you are taking vitamins with iron, resume these as tolerated.
- Do not smoke, as smoking delays healing and increases the risk of complications.
- Refrain from sleeping on your stomach for 3 weeks
Incision Care
- If drainage tube(s) have been placed, you may shower 48 hours after removal.
- Avoid exposing scars to sun for at least 12 months.
- Always use a strong sunblock, if sun exposure is unavoidable (SPF 30 or greater).
- Keep steri-strips on; replace if they come off (if applicable).
- Keep incisions clean and inspect daily for signs of infection.
- No tub soaking while sutures or drains are in place.
- You may pad the incisions with gauze for comfort.
- Wear garments (bra, ace wrap, taping) as directed by surgeon.
- Do NOT wear underwire bra.
What To Expect
- Expect some drainage onto the steri-strips (if applicable) covering the incisions.
- You are likely to feel tired for a few days, but you should be up and around in 4-5 days.
- Maximum discomfort will occur in the first few days after surgery.
- You may experience some numbness of nipples and operative areas.
- You may experience a burning sensation in your nipples for about 2 weeks.
- You may experience temporary soreness, tightness, swelling and bruising as well as some discomfort in the incision area.
- Your breasts may be sensitive to stimulation for a few weeks.
How Much Pain Is Ok?
How much breast, suture or incision pain is normal or ok? Proper healing is a key component in successful breast implant surgery. The worst of your breast augmentation recovery pain should subside a few days after surgery, but plan to spend weeks adjusting to the growing pains associated with breast implants – breast tightness, back pain.
Typically
- 1-2 days: You will feel the most pain, but meds help reduce it.
- 3-7 days: You will still feel sluggish and should still take it easy.
- 8-21 days: You will be sore but can get around more easily.
Women recovering from breast augmentation surgery often describe feeling a certain amount of discomfort, pain and tenderness across their breasts and along suture and incision line.
Dealing with sutures and incisions can be one of the most difficult aspects of recovery. When you feel the itch, you know your body’s healing, but don’t scratch. Excessive itchiness is not good. Ask you the office or Dr. Roesner for tips in handling excessive itchiness – should it occur.
Appearance
- Most of the discoloration and swelling will subside in 4-6 weeks.
- Your breasts may appear to ride high, but will drop over time as swelling subsides and the implant settles in.
- Scars may be red and angry looking for 6 months. In time, these usually soften and fade.
How Long Does It Take For Breast Implants To Settle In?
At your consult, you will discuss your health and lifestyle, review your medical history and determine your breast implant needs. At this time, Dr. Roesner can roughly estimate recovery time.
Your implants will need time to settle into their final position. The American Society for Aesthetic Plastic Surgery sets the following general time table for implant settling:
- 1 month: Most of the discoloration and swelling will subside in 4-6 weeks, implants begin to settle into position.
- 3-4 months: Implants reach a resting point.
- 8-12 months: Breasts fully settle.
In the interim, it may appear as if one breast implant is settling in more slowly or quickly than the other – or as if they’re both still sitting relatively high. Give them time, and don’t be alarmed. Initial asymmetry typically corrects itself with time.
Follow-up Care
- Sutures will be dissolvable. They are under your skin and released at the end of each incision. They are clear in appearance and will be trimmed to the skin line in 1-2 weeks.
- Continue with routine mammograms at a radiology center where technicians are experienced in the special techniques required with implants.
When to call
Signs you may not be recovering appropriately:
- Unusual discharge at incision points
- If you have any yellowish or greenish drainage from the incisions or notice a foul odor.
- Extreme nausea, vomiting or dizziness
- Numbness or tingling elsewhere in your body
- If you have loss of feeling or motion
- Severe itchiness at incisions, stitches or sutures
- If you have increased swelling or bruising.
- If swelling and redness persist after a few days.
- If you have increased redness along the incision.
- If you have severe or increased pain not relieved by medication.
- If you have any side effects to medications; such as, rash, nausea, headache, vomiting.
- If you have an oral temperature over 100.4 degrees.
- If you have bleeding from the incisions that is difficult to control with light pressure.
- Irregular heartbeat, chest pain or shortness of breath
For medical questions, please Contact us At (303) 440-7546
Possible Complications of Breast Augmentation Surgery
What are the potential risks of the surgery?
Women with sagging breasts, which is called “ptosis”, can also receive breast implants. Depending on how much the breast sags, an additional surgery may also be necessary. For breasts with nipples that droop below the lower crease of the breast, a breast lift surgery, or mastopexy, is often required as well. This surgery will also add scars around the nipple unlike most breast augmentation surgeries. Without this additional surgery to remove excess skin, placement of the implant can cause the breast to have a “double bubble” look. Commonly, women with sagging breasts often have the implants placed under the breast tissue, or “subglandular” to avoid these problems..
Early
1. Hypertrophic Scarring – This is a very thick, raised, red scar that develops after surgery. Hypertrophic scarring occurs in 2%-5% of patients and may require treatment with additional operations or steroid injections into the scar.
2. Hematoma – A hematoma is a pocket of blood inside the wound. It occurs in 1%-6% of patients and is usually occurs within 2-3 days after surgery. Hematoma symptoms are swelling of the breast and severe pain that does not respond to pain pills. Treatment includes putting a tube in the breast to drain the blood. This procedure often requires a trip back to the operating room. Sometimes, if the collection of blood is small, no treatment is required and the body is able to clear the hematoma on its own.
3. Seroma – In the days or weeks following the surgery, fluid can collect around the implant, causing pain or swelling. This can be thought of as “blister fluid.” Just like a hematoma, it can leak from vessels damaged during the surgery and form a collection. Removal of larger seromas is recommended since they can become infected. Usually, the fluid can be removed carefully by a needle and does not require additional surgery. However, this technique of draining the seroma with a needle also may create a hole in the implant leading to implant deflation.
4. Wound Separation (Dehiscence) – A relatively rare complication within the first 2 weeks where the edges of the wound separate resulting in an open wound or possibly exposure of the implant. This can be solved by using Steristrips to close the incision, or may require additional surgery.
5. Infection (Cellulitis) – This complication occurs in 2%-4% of patients, and is usually from bacteria that normally live on the skin. Most surgeons will give a single dose of antibiotics before the surgery, and use an antibiotic solution in the wound before implant placement to help reduce the chance of infection. Symptoms of infection include pain, redness, swelling, and fever. Doctors may treat this complication with antibiotic pills, or if the infection is severe, by having the patient go to the hospital for intravenous antibiotics until the swelling and redness go away. After leaving the hospital, antibiotics pills are taken for 1-2 weeks. For infections of the implant itself, surgery to remove the implant is often the only option. Though some surgeons will attempt to save the implant from being removed by reopening the pocket and washing out the wound, this may not be effective. Infected implants put the patient at additional risks including: scar contracture, wound separation, and (in very rare cases) a severe illness called Toxic Shock Syndrome. After removal, healing and softening of the breast need to take place before the implant can be replaced – which often takes several months.
6. Mondor’s Disease – This is an inflammation of the blood vessels that run under the surface of the breast and it occurs in about 1% of patients. Fortunately, this condition requires no additional treatment and will go away on its own.
Late
1. Asymmetry (difference in size or shape between breasts) – Most breast are asymmetric before breast augmentation, and all breasts remain (at least to some degree) asymmetric after the operation. Usually, the differences between the breasts can be improved during surgery, but occasionally the breast can become even more asymmetric after the operation and additional surgery may be required to improve this problem. For problems with sinking implants or implants placed off center, the wound is opened and the implant is moved. Sometimes if the first procedure is done in a subglandular approach, fixing the asymmetry can be done with submuscular implant placement.
2. Contour problems – These may be seen before or after breast augmentation. Although implants usually improve breast shape, contour irregularities may persist or worsen after the operation requiring additional surgery to correct them.
3. Capsular Contracture –
o Definition – Once an implant has been placed, cells called fibroblasts make scar tissue to surround the surface of the implant. This occurs around every implant in the body, including artificial joints, pacemakers, or shunts. The scar tissue that forms around the implant is called “connective tissue” or the “fibrous capsule” and is responsible for keeping the implant in place. This capsule, for reasons which are poorly understood, can sometimes thicken and contract. This squeezing of the implant can cause shape changes, hardening, or pain.
o Preventing Contracture – A number of factors may reduce the occurrence of capsular contracture. These include submuscular implant location, use of textured implants, and prevention of post-operative infection or bleeding. Sometimes doctors will also ask patients to start massaging the breast 5 days after surgery to reduce hardening of the capsule surrounding the implant. It should be noted, however, that massaging with textured implants is discouraged.
o Treatment For Capsulars Contracture – For severe capsular contractures, the treatment of choice is re-operation. During this procedure, scar tissue lining the implant pocket is removed. Subglandular implants may be moved to a submuscular position.
4. Altered Sensation or Feeling – Most women have some decrease of breast/nipple feeling or sensation following surgery. For women with these changes, feeling often returns after 6-12 months. Unfortunately, 15% of patients have loss of nipple sensation in at least one of their breasts. Loss of feeling to areas besides the nipple is common as well, though within a year most patients return to normal. Rarely, symptoms such as itching and tingling occur, but like the others, these normally end in 6 months.
5. Deflation or Rupture – The rate of deflation was published in one large, well-controlled study at 8.3%, though in the past this has often been a largely debated number. Implants that are placed in the subglandular position and implants larger than 450cc are at greatest risk for deflation. If this complication occurs, additional surgery is required to replace the implant. The cost of replacement usually is the responsibility of the patient.
Breast Implant Massage Exercises
It may be recommended that you perform breast implant massage or compression exercises.
In general, these exercises involve pushing the implant to the outermost corners of the pocket several times in succession. You move the implant up, down, to the right, and to the left. Hold your implant in each position for a few seconds. These exercises may help decrease your risk of developing capsular contracture (scar tissue around the implant).
You may be asked to start the exercises about a week after your breast implant surgery. ONLY perform massage exercises if instructed.
We recommend
- 10 cycles 2x/day for 6 week
- 10 cycles 1x/day indefinitely
Schedule your Appointment
And Meet Directly With Dr. Roesner to Discuss a Treatment plan to meet your Aesthetic and Skincare Goals.
Schedule AppointmentConsult fee is $100 – which will be applied to the cost of the procedure
(If scheduled within 90 days).